Vascular Access Management
Vascular access management is the comprehensive category of products, solutions and services providing a continuum of vascular access care, from patient assessment to device removal, designed to reduce vascular access related complications.


- Overview
- Resources
- Partner with BD
Up to 90% of hospital inpatients require IV therapy1
From insertion to removal, vascular access devices could see more than 200 touches
Every vascular access patient's journey is unique and full of variables:
- Multiple products to insert, care and maintain the device
- Many clinicians across shifts and care settings with varying skill levels and therapy goals
Vascular access complications can occur at many stages
Intravenous therapy is so common that it may be easy to forget there is potential for harm. Problems may arise when placing a vascular access device, from infections and occlusions, to dislodgement and phlebitis. These complications are a major cause of vascular access device failure. By better understanding the potential for risk, you can be better prepared to prevent patient complications.
A catheter-related bloodstream infection (CRBSI) is when the catheter is identified as the source of the infection.2* Signs and symptoms to look for include erythema; edema; any pain or tenderness or drainage and/or fever.2** There are extraluminal and intraluminal areas that could be potential spots for contamination, leading to CRBSIs from risk of breaking asepsis during insertion or care and maintenance; seeding bacteria from another site of infection; and ingress of bacteria due to non-intact dressing or suboptimal insertion site.3*
2*. Infusion Therapy Standards of Practice. J Infus Nurs. 2016; 39(1S): S147.
2**. Infusion Therapy Standards of Practice. J Infus Nurs. 2016; 39(1S): S106.
3*. Safdar N, Maki DG. Int Care Med. 2004; 30(1): 65.
When a catheter is blocked, this can either prevent infusion or injection of solution into a catheter, aspirate blood from a catheter, or both.2* Signs and symptoms to look out for include sluggish flow and/or blood return, inability to withdraw blood, flush and/or infuse through the catheter, frequent occlusion alarms on an electronic infusion device, and infiltration or extravasation or swelling and/or leaking at the infusion site.2** Occlusions may be caused by multiple factors, including allowing an infusion to run dry, improper flushing, infusing incompatible medications, or employing an improper clamping sequence.2**
2*. Infusion Therapy Standards of Practice. J Infus Nurs. 2016; 39(1S): S153.
2**. Infusion Therapy Standards of Practice. J Infus Nurs. 2016; 39(1S): S104.
Catheter movement into or out of the insertion site indicating tip movement to a suboptimal position.2* Signs and symptoms include the inability to continue infusion, increased external catheter length since previous assessment and leakage at insertion site. Additionally, if the catheter moves out of the vein but not the skin, it can result in edema, pain, changes in skin color and even progress to blistering and ulceration.2** Risk factors to consider include poor site selection, loosening of the catheter due to inadequate stabilization and lack of proper securement, as well as patient manipulation such as arm or body movement.2†
2*. Infusion Therapy Standards of Practice. J Infus Nurs. 2016; 39(1S): S147.
2**. Infusion Therapy Standards of Practice. J Infus Nurs. 2016; 39(1S): S91.
2†. Infusion Therapy Standards of Practice. J Infus Nurs. 2016; 39(1S): S116.
Inflammation of a vein2* could be evident by pain and tenderness, erythema, warmth, swelling and redness at the catheter site.2** There are multiple chemical, mechanical and bacterial issues that could be the cause. These include use of irritating solutions, not allowing skin antisepsis to dry, inadequate hemodilution, improper catheter size or stabilization techniques, breaks in aseptic technique or non-occlusive dressing.2**
2*. Infusion Therapy Standards of Practice. J Infus Nurs. 2016; 39(1S): S153.
2**. Infusion Therapy Standards of Practice. J Infus Nurs. 2016; 39(1S): S95.
Infiltration occurs when a nonvesicant solution or medication is inadvertently administered into tissue surrounding the catheter site, whereas extravasation occurs when the solution or medication is vesicant.2* When this occurs, the patient may suffer from edema, pain, changes in skin color and fluid leakage from the catheter insertion site, additionally extravasation may progress to blistering and ulceration.2** A myriad of issues may cause infiltration or extravasation, including inappropriate insertion site, inadequate stabilization, difficult access history, medications that alter pain sensation, disease that produces change in vasculature, use of deep veins with insufficient catheter length, and the inability of the patient to report their symptoms.2†
Partner with BD to assess your vascular access risk
Download the Challenges of Vascular Access Infographic
2*. Infusion Therapy Standards of Practice. J Infus Nurs. 2016; 39(1S): S150, S149.
2**. Infusion Therapy Standards of Practice. J Infus Nurs. 2016; 39(1S): S99.
2†. Infusion Therapy Standards of Practice. J Infus Nurs. 2016; 39(1S): S98.
Infections caused by resistant organisms are associated with high mortality rates and costs compared to those susceptible to antimicrobial therapy.
Delays in appropriate diagnosis and treatment increase the chances of a negative clinical outcome for patients with these infections.5
This calculator quantifies the estimated clinical and economic impact of antimicrobial resistance.
Calculate the cost of CLABSIs in your facility:
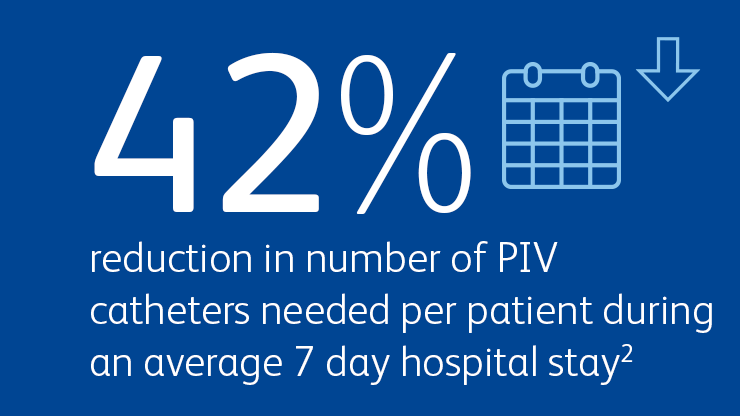
Calculate the cost of PIVC restarts in your facility:
Helping patients on the vascular access continuum
As a clinician, you’re often tasked to perform one of the most common invasive procedures—placing a vascular access device. With the right training and knowledge, you may potentially reduce vascular access complications and improve patient outcomes. And we’re here to help, every step of the way.
- Calculate the potential costs of complications
- On average, CLABSIs cost $45,814 per patient occurence4
- Unnecessary, peripherally inserted venous catheter (PIVC) restarts can cost a 200-bed hospital more than $980,000 annually
An integrated solution that may help improve vascular access care
An integrated solution that may help improve vascular access care
You are a caregiver whose role is to provide patients with a positive experience and the best possible care.
Your challenges and how BD can help:
When placing IVs in difficult to access locations, multiple attempts can be stressful and impact the patient experience.
- We provide an extensive collection of online clinical practice training and education modules designed to support ongoing enrichment in vascular access, insertion and care.
Staying up to date on current evidence-based practices in vascular access as healthcare continues to evolve rapidly.
- Our extensive portfolio of vascular access devices, paired with product training and education, can help you address the vascular access needs of all patients.
Finding targeted continuing education resources quickly that meet your developmental needs.
- We partner with key opinion and clinical thought leaders to create and share webinars on the latest data and insights.
You are a clinical decision-maker whose role requires rapid pairing of patient IV therapy needs with the right vascular access devices.
Your challenges and how BD can help:
Delays in patient treatment can affect efficiencies, so you need staff to be confident in gaining and maintaining vascular access in patients.
- Our clinical training and education programs provide information on proper vascular access device selection, placement and complication management.
Changes in science and technologies require you to stay up to date on the latest information for optimal patient care.
- We are here to support you with evidence-based resources.
Changes in staff or frequent turnover can create variation and gaps between best practices and current practice.
- Our customer assessment and recommendation program may help reduce variation while providing visibility into discord between practice and policies.
You are the leader responsible for key imperatives that enhance employee engagement, while improving operational, financial and clinical outcomes.
Your challenges and how BD can help:
Finding and tracking gaps in vascular access clinical practice that may be negatively making an impact on patient experience and/or economic outcomes.
- Our customer assessment and recommendation program can improve visibility into gaps between policies and practice, which may be exposing your organization to risk.
Arming your team with on-demand training and education resources in a fast-paced industry where clinical practice continues to evolve.
- We offer evidence-based resources and continuing education to support your staff in elevating your vascular access programs.
You are a clinical leader who is passionate about reducing risks of healthcare-acquired infections (HAIs) and improving overall quality of care.
Your challenges and how BD can help:
Addressing and reducing risks of HAIs in your facility while ensuring patient care is not being compromised due to lack of consistency of best practices.
- Our customer assessment and recommendation program can improve visibility into gaps between policies and practice, which may be leading to vascular access complications.
Staying up to date on the latest technologies and best practices in preventing HAIs as science continues to evolve.
- We offer the latest insights and evidence-based practices from key opinion leaders (KOLs) in our library of webinars and resources.
Changing staff and frequent clinician turnover can create variation in knowledge and expertise resulting in gaps in clinical practice.
- Our on-demand training and education programs support development for clinicians at all levels and can help your facility sustain adherence to vascular access best practices.
You are responsible for managing relationships with the vendor whose products help standardize practice and improve clinical outcomes while maintaining your hospital's economic goals.
Your challenges and how BD can help:
Acquiring information about the latest vascular access innovations that provide both financial efficiencies and improved patient outcomes.
- We can provide insight into the financial and clinical implications of implementing new technologies with our library of data and resources.
Understanding key attributes of vascular access devices that provide both positive patient and economic outcomes.
- Our extensive portfolio of vascular access products is accompanied by a support team that can help you make informed decisions.
You are a clinical leader responsible for developing educational programs appropriate for your clinicians of varying levels of experience and understanding.
Your challenges and how BD can help:
Developing ongoing clinical training and education programs appropriate for clinicians of varying levels of experience and understanding.
- Our on-demand training and education programs can support you in elevating your vascular access best practice programs.
Staying up to date on the latest technologies and best practices in vascular access in an industry where practice continues to evolve.
- We offer a library of clinical resources to help you expand your own knowledge while enhancing your training and education programs.

Solution 01 Solution 01

Solution 01 Solution 01

Solution 01 Solution 01

Solution 01 Solution 01
- Helm RE, Klausner JD, Klemperer JD, Flint LM, Huang E. Accepted but unacceptable: peripheral IV catheter failure. J Infus Nurs. 2015;38(3):189-203.
- Infusion Nurses Society. Infusion Nursing Standards of Practice. J Infus Nurs. 2016;39(1S):S1-S159.
- Safdar N, Maki DG. The pathogenesis of catheter-related bloodstream infection with noncuffed short term central venous catheters. Int Care Med. 2004;30(1):62-67. doi: 10.1007/s00134-003-2045-z
- Zimlichman E, Henderson D, Tamir O, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 2013;173(22):2039-2046. doi:10.1001/jamainternmed.2013.9763
-
 Learn more
Learn moreMy BD Learning for additional training and educational resources
(Use activation code: BDclinical)
Infusion Therapy Practice training videos
Hand Hygiene video
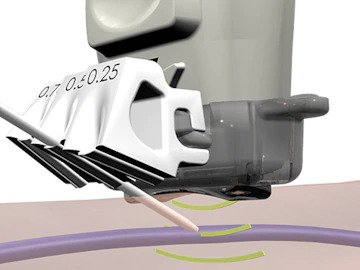
PIVC Insertion video
PIVC Dressing Change video
PIVC Removal video
Continuous Infusion video
IV Push Infusion video

6 Benefits of incorporating standards of practice into your vascular access management program

Hospital Acquired Conditions (HAC) Reduction Program, Your Frequently Asked Questions Answered

What are Vascular Access-Associated Bloodstream Infections? Some Key Facts Hospital Staffs Should Know
- Helm RE, Klausner JD, Klemperer JD, Flint LM, Huang E. Accepted but unacceptable: peripheral IV catheter failure. J Infus Nurs. 2015;38(3):189-203.
- Infusion Nurses Society. Infusion Nursing Standards of Practice. J Infus Nurs. 2016;39(1S):S1-S159.
- Safdar N, Maki DG. The pathogenesis of catheter-related bloodstream infection with noncuffed short term central venous catheters. Int Care Med. 2004;30(1):62-67. doi: 10.1007/s00134-003-2045-z
- Zimlichman E, Henderson D, Tamir O, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 2013;173(22):2039-2046. doi:10.1001/jamainternmed.2013.9763
Address gaps in your vascular access process with four steps
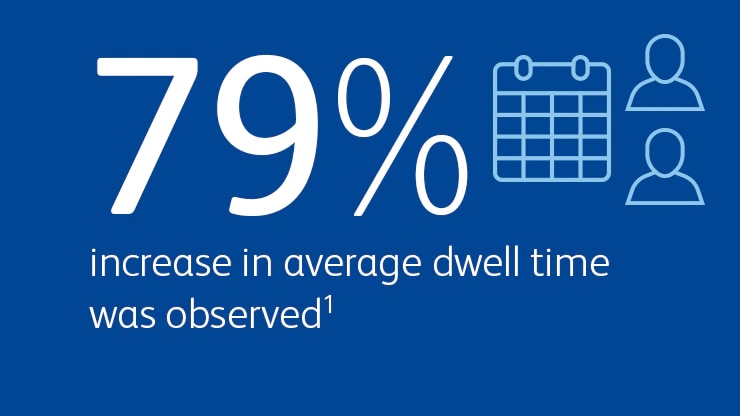
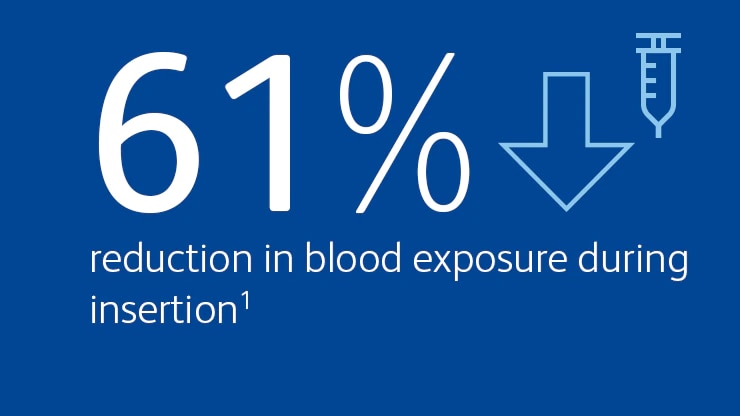
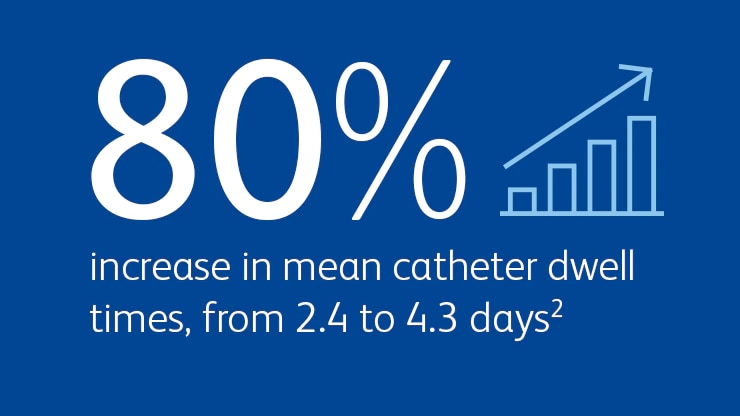
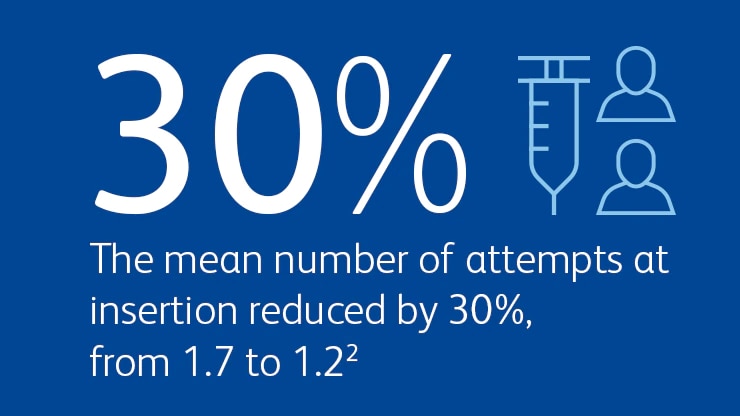
With our help, you may see improvements in clinical outcomes with BD products, such as reduction in blood exposure during insertion, increased average dwell time of peripheral IVs and decreased vascular access complications, additionally, your facility could benefit from economic efficiencies with enhanced protocols and best practices.
-
Assess and recommend
Our experienced clinical experts will perform a comprehensive assessment of BD products and clinical practice across your facility, leveraging proprietary digital tools, which will help in developing insightful data.
-
Identify and implement
Lean about and evaluate our comprehensive portfolio of products.
-
Train
Our clinical teams collaborate with your facility's leadership to develop curricula that addresses your unique BD product training needs, while supporting evidence-based policies and procedures.
-
Share
Gain insights from your peers' vascular access success stories and share your own
BD Vascular Access Program Assessment
You can't see how far you've come unless you know where you began. Our experienced clinical experts will perform a comprehensive assessment of BD products and clinical practice across your facility, leveraging proprietary digital tools, which will help in developing insightful data.
Once completed, we'll provide a detailed, actionable road map to help you standardize and align best practices across the vascular access continuum.
-
Clincian Interviews
-
Vascular site Assessments
-
Chart and Policy reviews
-
Clinical Practice Observations
Request an assessment
Comprehensive portfolio of products
Since we are a global leader in vascular access devices, you can be confident that the products you are using are engineered to the highest quality and safety standards, backed by years of development and healthcare use. Our goal is to help you provide the best possible care at every step in the vascular access continuum.
Learn more about our technologies and products
Expert BD clinical training and education
Our clinical teams collaborate with your facility's leadership to develop curricula that addresses your unique BD product training needs, while supporting evidence-based policies and procedures. With a solid educational program in place, you can maintain best practices, which leads to repeatability and sustainability for continuity.
- Morrell E. Reducing risks and improving vascular access outcomes. J Infus Nurs. 2020;43(4):222-228. doi:10.1097/NAN.0000000000000377
- Platt V, Osenkarski S. Improving vascular access outcomes and enhancing practice. J Infus Nurs. 2018;41(6):375-382. doi:10.1097/NAN.0000000000000304